Ovarian Pathology
Polycystic Ovarian Syndrome
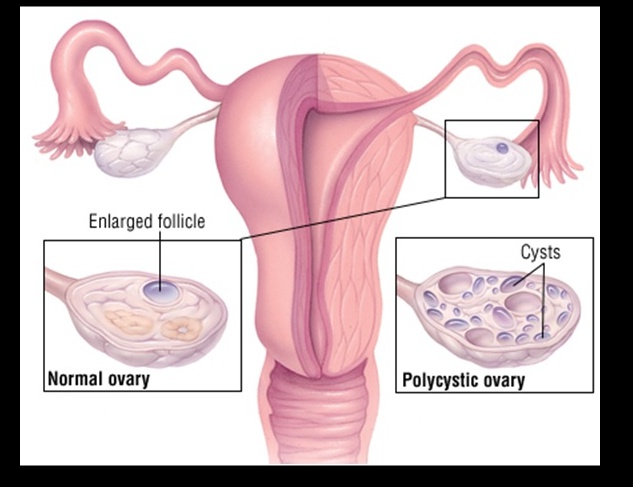
(Stein-Leventhal Syndrome) is a condition that affects roughly 5% of women of reproductive age, and is characterized by the formation of multiple ovarian follicular cysts due to hormone imbalance.
Pathogenesis
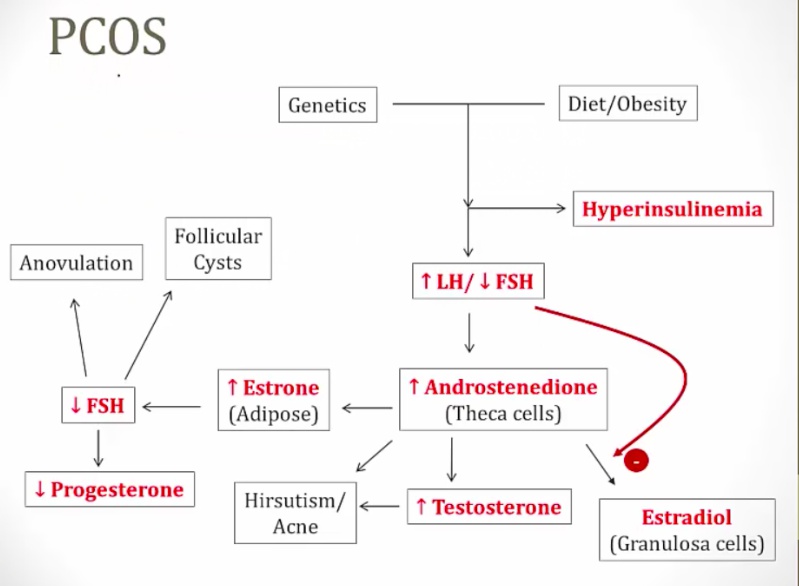
The pathogenesis of polycystic ovarian syndrome in general is poorly understood, however the following is the current understanding:
- Caused by genetics + diet and obesity
- High amplitude GnRH pulses lead to increased pituitary release of LH. This stimulates increased androgen synthesis by the theca cells in the ovary, resulting in increased androgen aromatization to estrone in peripheral adipose tissue. The high level of circulating estrone exerts a negative feedback on FSH release from the pituitary gland. FSH is needed for proper maturation of the developing follicle, and these low levels of FSH result in cystic degeneration of the follicle
- Result: secondary amenorrhea and anovulation
Polycystic ovarian disease is also related to the development of insulin resistance:
- Insulin stimulates theca cell secretion of androgens and the inhibition of hepatic sex-hormone binding globulin production. This increases free androgens and also increases androgen aromatization to estrone in peripheral adipose tissue. In both cases, excess levels of androgen are being produced, aromatized to estrone or estradiol, and then exerting negative feedback on FSH secretion.
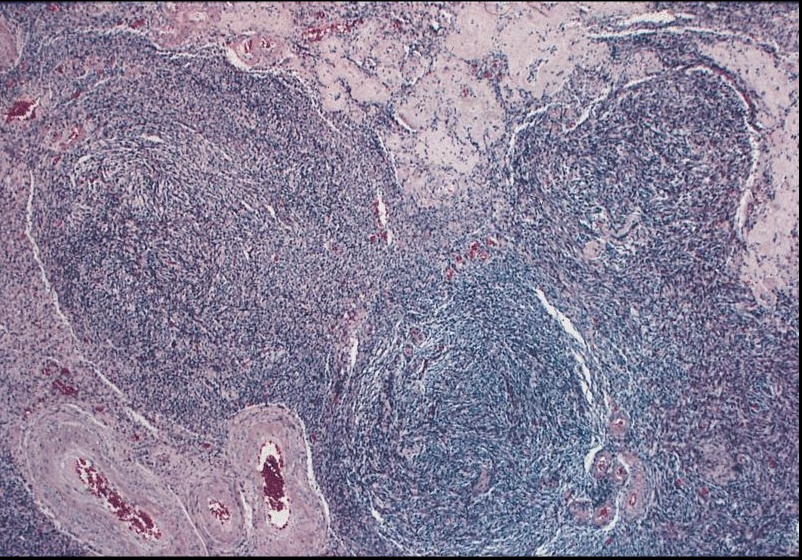
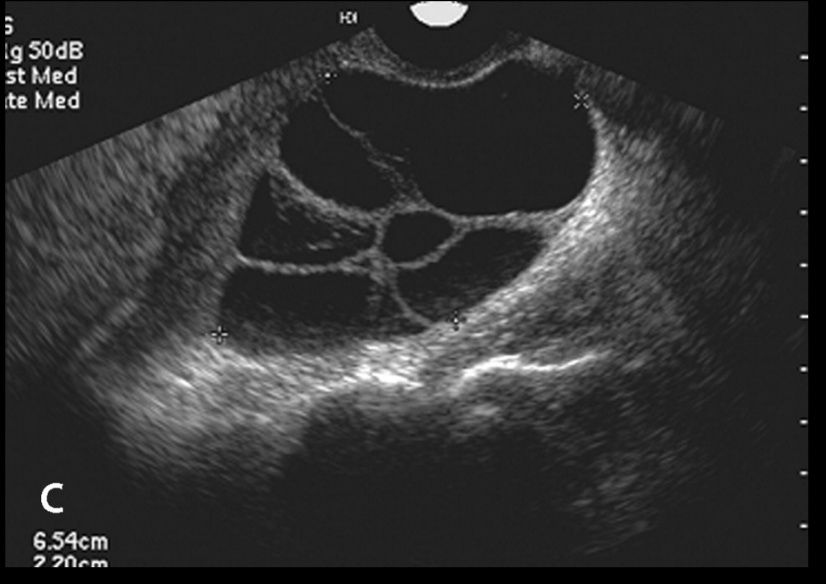
The decreased secretion of FSH from estrone negative feedback leads to follicular degeneration and subsequent fluid-filled cyst formation. This continues to occur with each cycle, and leads to the formation of ovaries with multiple degenerating cysts (hence polycystic).
Symptoms and Presentation
Symptoms include:
-
Increased testosterone: The increased release of free androgens leads to hirsutism (increase in hair) and virilism, a female disorder in which there is development of secondary male sexual characteristics, as hirsutism and lowered voice, caused by various conditions affecting hormone regulation. Acne
-
Suppression of FSH: secondary amenorrhea, infertility, multiple folicular cysts on ultrasound
-
Development of diabetes:
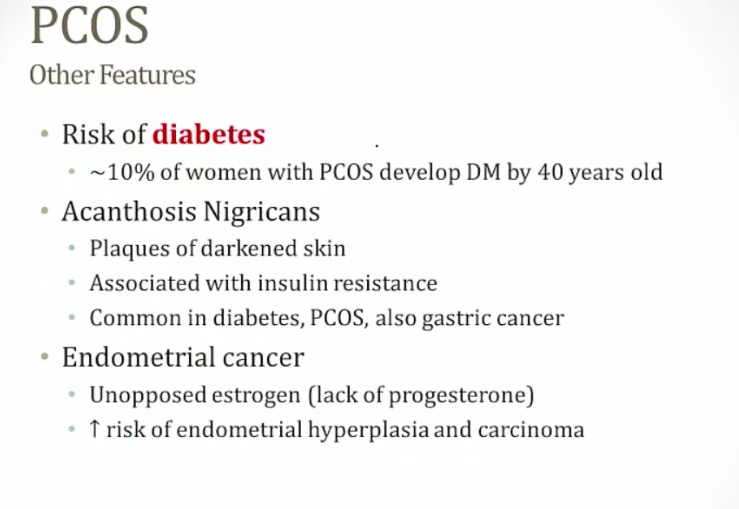
The classic presentation of a patient with polycystic ovarian syndrome is an overweight young woman presenting with infertility, oligomenorrhea and hirsutism. Some patients may also develop insulin resistance (seen in 50-70% of women with PCOS) leading to the development of type 2 diabetes mellitus 10-15 years later.
Women with PCOS experience prolonged exposure to unopposed, increased levels of estrone (no progesterone from corpus luteum) results in an increased risk of endometrial and breast cancer.
Diagnosis
Two out of three of the following criteria are required to make the diagnosis of PCOS:
- Oligomenorrhea
- Hyperandrogenism
- Polycystic ovaries on ultrasound
- **LH:FSH ratio > 2 **

Treatments
The treatment for polycystic ovarian syndrome includes the following:
- Oral contraceptives (OCPs) (primary treatment)
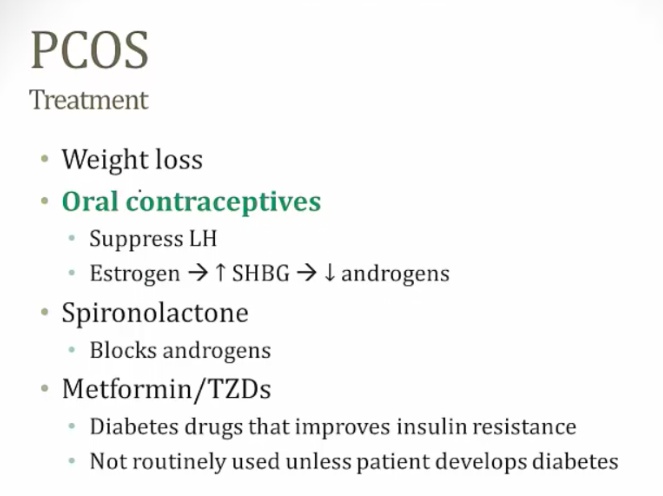
- Clomiphene citrate (used for women that desire to get pregnant)
Folicular Cyst
Follicular Cyst development occurs when fluid accumulates within either the Graafian (mature) follicle or a previously ruptured follicle.
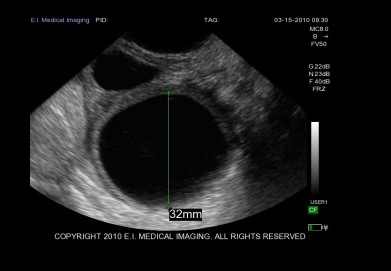
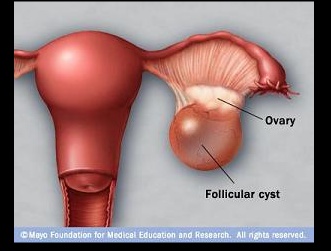
Most common ovarian mass overall.
Rupture of a follicular cyst often presents with sudden pain and sterile peritonitis.
Follicular cysts are associated with hyperestrogenism. Decreased FSH secretion from negative estrogen feedback leads to follicular degeneration
Corpus Luteum Cyst
Corpus Luteum Cyst development occurs when **fluid (e.g. blood) accumulates within the corpus luteum during pregnancy. ** (early pregnancy especially)
Top: corpus luteum, yellow. Bottom: ovary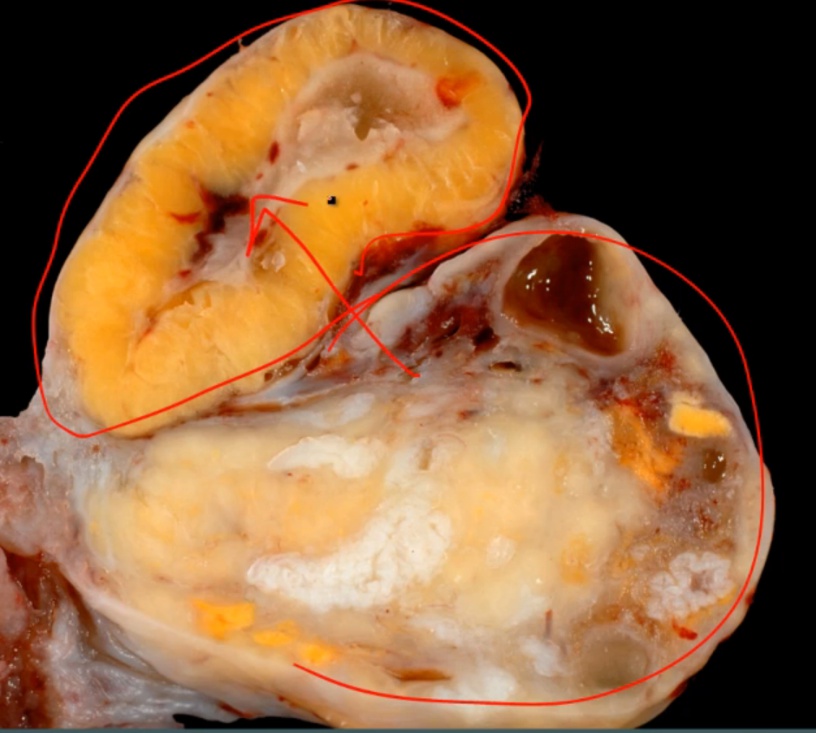
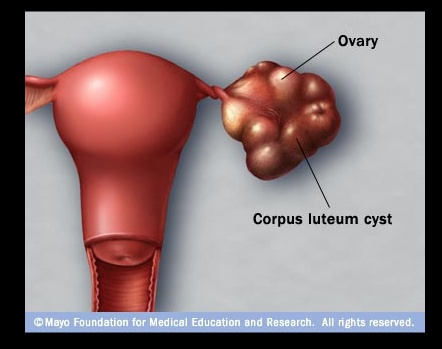

The most common ovarian mass during pregnancy, and most regress spontaneously.
Theca-Lutein Cyst
Theca-Lutein cysts develop from excessive gonadotropin stimulation. They will often be accompanied by abnormally high levels of beta-hCG and high levels of androgens.
Characterized by cysts lined by luteinized theca cells. Theca-Lutein cysts are often multiple and bilateral.
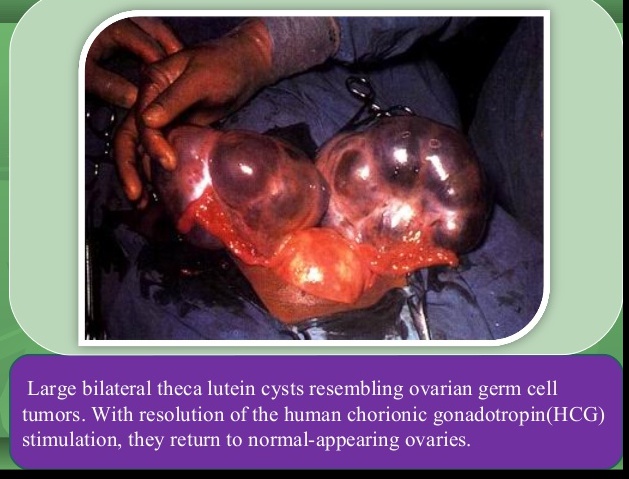
Very high association with gestational trophoblastic disease, such as choriocarcinoma and hydatidiform moles.
Stromal Hyperthecosis
Benign bilateral ovarian enlargement that is most commonly seen in obese postmenopausal women. Stromal hyperthecosis is also associated with metabolic syndrome and acanthosis nigricans.
Characterized by hyperplasia of the theca interna of the ovary, which results in excess androgen production by luteinized cells. This leads to hirsutism and virilization(masculinization).